Are you considering alternative health insurance options for your business? Self-funded health insurance has emerged as a compelling choice for employers seeking greater control over their healthcare costs and benefits design. But is it the right fit for your organization?
As an experienced benefits consultant who has guided countless businesses through this decision, I’ve seen firsthand how self-funded plans can transform a company’s approach to employee healthcare. The potential for significant cost savings and customization is real—but so are the risks and responsibilities that come with this model.
In this comprehensive guide, we’ll explore everything you need to know about self-funded health insurance pros and cons, from its fundamental mechanics to the critical advantages and potential drawbacks that could impact your business. Whether you’re a small business owner curious about alternatives to traditional insurance or a benefits manager evaluating options for a growing company, this article will equip you with the knowledge to make an informed decision.
TL;DR - Self-Funded Health Insurance Pros and Cons
Self-funded health insurance allows employers to directly assume financial responsibility for employee health claims instead of paying premiums to an insurance carrier. The major advantages include potential cost savings (up to 15-30% in some cases), complete claims transparency, customizable benefits packages, and greater control over healthcare spending. However, this approach comes with significant challenges: financial risk from unexpected high-cost claims, administrative complexity, regulatory compliance requirements, and the need for specialized expertise. While traditionally favored by larger organizations, innovative solutions now make self-funding increasingly accessible to small and mid-sized businesses. The decision ultimately depends on your organization’s financial stability, risk tolerance, employee demographics, and administrative capabilities.
What is Self-Funded Health Insurance?
Self-funded health insurance, also known as self-insured health plans or Administrative Services Only (ASO) arrangements, is a healthcare financing model where employers directly assume the financial responsibility for their employees’ health benefit claims. Unlike traditional fully-insured plans where companies pay fixed premiums to insurance carriers, self-funded employers set aside their own funds to pay employee healthcare claims as they occur.
In a self-funded arrangement, the employer establishes a special trust or account from which to pay claims. This fund is typically built through a combination of employer contributions and employee payroll deductions. When an employee receives medical care, instead of an insurance company paying the provider, the payment comes directly from this dedicated fund.
How Self-Funded Health Insurance Works
The mechanics of self-funded health insurance involve several key components:
- Plan Design: The employer, not an insurance company, determines the specific benefits offered, including covered services, exclusions, deductibles, copayments, and other plan features.
- Claims Administration: Most employers partner with a Third-Party Administrator (TPA) to process claims, provide customer service, and handle day-to-day plan operations. Some insurance companies also offer these administrative services without taking on the insurance risk.
- Provider Networks: Self-funded plans typically contract with provider networks to secure discounted rates for medical services, similar to traditional insurance plans.
- Stop-Loss Insurance: To protect against catastrophic claims, most self-funded employers purchase stop-loss insurance, which reimburses the employer for claims that exceed predetermined thresholds. This coverage comes in two forms:
- Specific (Individual) Stop-Loss: Protects against unexpectedly high claims from any single plan member
- Aggregate Stop-Loss: Protects against higher-than-expected claims across the entire plan
- Regulatory Framework: Self-funded plans are governed primarily by federal law (ERISA) rather than state insurance regulations, which provides certain advantages in terms of plan design flexibility and consistent multi-state administration.
Self-Funded vs. Fully-Insured: Key Differences
| Feature | Self-Funded Plans | Fully-Insured Plans |
|---|---|---|
| Financial Risk | Employer bears primary risk (4/5) | Insurance carrier bears risk (2/5) |
| Premium Taxes | Exempt from state premium taxes (5/5) | Subject to state premium taxes (2-3%) (2/5) |
| Regulatory Burden | Primarily federal (ERISA) (4/5) | Both federal and state regulations (2/5) |
| Cash Flow | Pay claims as they occur (5/5) | Pay fixed premiums in advance (2/5) |
| Plan Design | Highly customizable (5/5) | Limited to carrier offerings (2/5) |
| Data Access | Complete claims transparency (5/5) | Limited data access (1/5) |
| Administrative Control | Higher (often outsourced to TPA) (5/5) | Lower (handled by carrier) (2/5) |
Based on industry averages and regulatory requirements. Ratings indicate relative advantage (higher is better).
Who Typically Uses Self-Funded Health Insurance?
Historically, self-funding was primarily adopted by large corporations with thousands of employees, as their large employee pools provided statistical predictability for claims. However, the landscape has evolved significantly:
- According to the Employee Benefit Research Institute, approximately 64% of US workers with employer-sponsored health coverage are now in self-funded plans
- While still most common among large employers (91% of those with 5,000+ employees), self-funding has gained traction with mid-sized companies (67% of those with 200-999 employees)
- Even small businesses are increasingly exploring self-funded insurance options through innovative arrangements like level-funding (a hybrid approach) and captive insurance programs
This shift reflects growing employer interest in controlling healthcare costs, gaining transparency into claims data, and customizing benefits to meet workforce needs.
Major Advantages Of Self-Insurance For Businesses
Self-funded health insurance offers several compelling advantages that have made it increasingly popular among businesses of all sizes. These benefits extend beyond simple cost considerations to include greater control, flexibility, and data-driven decision-making capabilities.
Significant Cost Savings Potential
Perhaps the most attractive aspect of self-funding is the potential for substantial cost savings:
- Elimination of Insurance Carrier Profit Margins: Traditional insurance carriers typically build a 3-5% profit margin into their premiums. Self-funding eliminates this expense entirely.
- Avoidance of State Premium Taxes: Self-funded plans are exempt from state premium taxes, which typically range from 2-3% of premium costs. For a company spending $1 million on healthcare, this alone could represent $20,000-$30,000 in annual savings.
- Cash Flow Advantages: Rather than paying premiums in advance, self-funded employers pay claims as they occur, allowing them to retain and invest funds until needed. This improved cash flow can generate additional interest income.
- Pay Only for Actual Claims: With traditional insurance, employers pay fixed premiums regardless of actual claims experience. In self-funded arrangements, employers only pay for claims that actually materialize. Studies show that in years with favorable claims experience, savings can range from 15-30% compared to fully-insured premiums.
Reduced Administrative Costs: While TPAs charge fees for administration, these costs are often lower than the administrative portion built into insurance premiums, particularly for mid-sized and large employers.
| Year | Fully-Insured Plan Cost | Self-Funded Plan Cost | Annual Savings | Cumulative Savings |
|---|---|---|---|---|
| Year 1 | $1,000,000 | $950,000 | $50,000 | $50,000 |
| Year 2 | $1,050,000 | $920,000 | $130,000 | $180,000 |
| Year 3 | $1,102,500 | $890,000 | $212,500 | $392,500 |
| Year 4 | $1,157,625 | $870,000 | $287,625 | $680,125 |
| Year 5 | $1,215,506 | $850,000 | $365,506 | $1,045,631 |
Based on a hypothetical company with 100 employees. Assumptions: 5% annual premium increase for fully-insured plan; Self-funded plan shows initial savings and improved cost management over time. Actual results may vary.
Complete Claims Transparency and Data Access
Self-funding provides unprecedented visibility into healthcare spending:
- Detailed Claims Data: Employers gain access to comprehensive claims information (appropriately de-identified to protect privacy), allowing them to understand exactly where healthcare dollars are being spent.
- Utilization Patterns: This transparency reveals which types of services are being used most frequently, which conditions are driving costs, and which providers are delivering care.
- Data-Driven Decision Making: With this information, employers can make informed decisions about plan design, wellness initiatives, and provider partnerships based on their specific population’s needs rather than industry averages.
Fraud Detection: Detailed claims review can help identify potential billing errors or fraudulent claims that might otherwise go unnoticed in a fully-insured arrangement.
Customized Plan Design and Flexibility
Self-funded health insurance offers unparalleled flexibility in designing health benefits:
- Tailored Benefits Package: Employers can customize coverage to meet the specific needs of their workforce rather than accepting one-size-fits-all insurance products.
- Targeted Wellness Programs: With claims data insights, employers can implement wellness initiatives that address their population’s actual health challenges.
- Provider Network Flexibility: Self-funded plans can contract with preferred providers or multiple networks to ensure employees have access to high-quality, cost-effective care.
- Regulatory Advantages: Self-funded plans are governed primarily by federal ERISA regulations rather than varying state insurance laws, providing greater consistency for multi-state employers and exemption from certain state mandates.
Rapid Adaptation: When healthcare needs change, self-funded employers can modify their plans more quickly than those with traditional insurance, which typically only allows changes during annual renewal periods.
Greater Control Over Healthcare Spending
Self-funding puts employers in the driver’s seat:
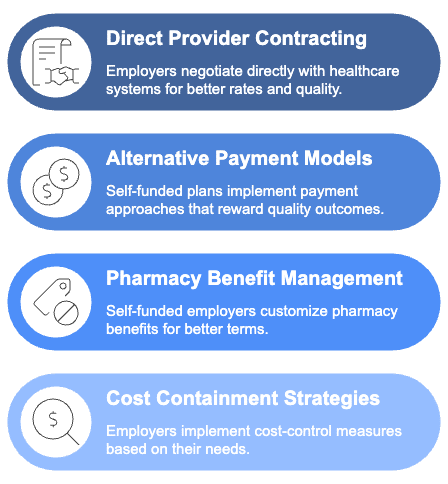
- Direct Provider Contracting: Some self-funded employers negotiate directly with healthcare systems or centers of excellence for specific procedures, securing better rates and quality guarantees.
- Alternative Payment Models: Self-funded plans can implement innovative payment approaches like reference-based pricing or value-based care arrangements that reward quality outcomes rather than service volume.
- Pharmacy Benefit Management: With rising prescription costs, self-funded employers can customize their pharmacy benefits, implement step therapy programs, or negotiate directly with pharmacy benefit managers for better terms.
Cost Containment Strategies: Employers can implement various cost-control measures such as care navigation services, second opinion programs, or telemedicine options based on their specific needs.
Real-World Success Stories
Many organizations have achieved remarkable results through self-funding:
- A mid-sized manufacturing company with 250 employees saved approximately $400,000 in the first year after switching to self-funding, representing a 22% reduction in healthcare spending.
- A regional retail chain implemented targeted diabetes management programs based on claims data insights, reducing emergency room visits by 30% and improving medication adherence among affected employees.
- A technology firm used self-funding flexibility to create a benefits package that emphasized mental health services and preventive care, reporting improved employee satisfaction and reduced absenteeism.
These advantages explain why self-funded health insurance continues to grow in popularity across the business spectrum, from large corporations to increasingly smaller organizations seeking greater control over one of their largest expense categories.
Critical Problems With Self-Funded Insurance Plans
While self-funded health insurance offers numerous advantages, it’s essential to understand the potential challenges and risks involved. Being aware of these issues allows employers to implement appropriate safeguards and determine if self-funding aligns with their risk tolerance and organizational capabilities.
Financial Risk and Volatility
The most significant concern with self-funding is the financial exposure:
- Catastrophic Claims Exposure: Without proper protection, a single catastrophic claim (such as a premature birth, organ transplant, or cancer treatment) can cost millions of dollars and severely impact an employer’s finances.
- Cash Flow Unpredictability: Unlike the predictable premium payments of fully-insured plans, self-funded claims can fluctuate dramatically from month to month, creating budgeting challenges.
- Reserve Requirements: Employers must maintain adequate reserves to cover expected and unexpected claims, which ties up capital that could otherwise be used for business operations or investments.
- Potential for Lasering: When renewing stop-loss coverage, insurers may “laser” (set higher attachment points for) specific high-risk individuals, increasing the employer’s financial exposure for those employees.
Year-to-Year Volatility: Smaller employers especially may experience significant swings in claims costs from year to year, making long-term financial planning more challenging.
Administrative Complexity and Burden
Self-funded insurance introduces administrative responsibilities that many employers aren’t equipped to handle internally:
- Claims Processing Infrastructure: Employers must establish systems for processing claims efficiently and accurately, typically requiring third-party assistance.
- Compliance Requirements: Self-funded plans must adhere to numerous federal regulations, including ERISA, HIPAA, ACA, and others, creating compliance obligations that require specialized knowledge.
- Plan Document Maintenance: Employers must create and maintain detailed plan documents that clearly outline covered benefits, exclusions, and administrative procedures.
- Appeals and Grievance Procedures: Self-funded plans must establish formal processes for handling member appeals and grievances in accordance with regulatory requirements.
- Vendor Management: Most self-funded employers work with multiple vendors (TPAs, stop-loss carriers, pharmacy benefit managers, etc.), requiring coordination and oversight.
Expertise and Resource Requirements
Successfully managing a self-funded plan demands specialized knowledge:
- Healthcare Analytics Capabilities: To fully leverage claims data, employers need staff or partners with healthcare analytics expertise to identify trends and opportunities.
- Actuarial Support: Determining appropriate funding levels and stop-loss attachment points typically requires actuarial analysis that most employers don’t have in-house.
- Healthcare Compliance Knowledge: Keeping up with evolving healthcare regulations requires dedicated resources or external support.
- Provider Network Management: Negotiating and maintaining provider relationships requires healthcare contracting expertise.
- Employee Communication Skills: Explaining the complexities of self-funded benefits to employees requires effective communication strategies.
Potential Employee Impact
Self-funding can affect the employee experience in several ways:
- Benefit Changes: The transition to self-funding may involve changes to benefits, networks, or administrative procedures that can create employee confusion or dissatisfaction if not properly communicated.
- Claims Processing Adjustments: Employees accustomed to a particular insurance carrier’s claims process may need to adapt to new procedures under a TPA.
- Perception Concerns: Some employees may worry about their employer having access to health information, even though HIPAA regulations strictly limit such access.
Continuity of Care: Changes in provider networks or formularies may disrupt ongoing care for some employees, requiring careful transition planning.
Mitigating the Challenges
While these challenges are significant, they can be effectively managed with proper planning:
- Comprehensive Stop-Loss Coverage: Appropriate specific and aggregate stop-loss insurance is essential for protecting against catastrophic claims and overall volatility.
- Experienced TPA Partnerships: Working with established, reputable TPAs can significantly reduce administrative burdens and compliance risks.
- Phased Implementation: Some employers transition gradually through level-funding or partial self-funding arrangements before moving to full self-funding.
- Employee Education: Clear, transparent communication about how the plan works helps address employee concerns and sets appropriate expectations.
- Expert Guidance: Working with experienced benefits consultants, brokers, and legal advisors who specialize in self-funding can help navigate complex decisions.
Understanding these challenges is not meant to discourage employers from considering self-funded health insurance, but rather to ensure they approach this option with realistic expectations and appropriate safeguards. With proper planning and expert guidance, many organizations successfully navigate these challenges and realize the substantial benefits that self-funding can offer.
| Consideration | Rating (1-5) | Explanation |
|---|---|---|
| Cost Savings | 4.2 | Self-funded plans typically offer significant cost savings through elimination of carrier profit margins, exemption from premium taxes, and improved cash flow management. |
| Risk Management | 3.8 | With proper stop-loss coverage and risk mitigation strategies, self-funded plans can effectively manage financial exposure while maintaining benefits. |
| Small Business Viability | 3.5 | While traditionally used by larger organizations, innovations like level-funding have made self-funding increasingly viable for smaller businesses with proper safeguards. |
| Regulatory Compliance | 3.6 | Self-funded plans face fewer state regulations but must comply with federal requirements like ERISA, ACA, and HIPAA, creating a mixed regulatory burden. |
| Administrative Burden | 2.9 | Self-funding requires more administrative oversight and expertise, though third-party administrators can manage much of this complexity for a fee. |
Based on industry expert assessments for average mid-sized businesses. Ratings indicate relative advantage (higher is better).
How to Decide If Self-Funded Health Insurance Fits Your Business
Making the decision to transition to self-funded health insurance requires careful consideration of your organization’s unique circumstances. This section will guide you through the key factors to evaluate when determining if self-funding is the right approach for your business.
Assessing Your Organization's Financial Stability
Financial readiness is perhaps the most critical factor in determining self-funding suitability:
- Cash Flow Analysis: Evaluate whether your business has sufficient cash reserves to handle the potential volatility of healthcare claims. Most experts recommend having at least three to six months of expected claims in reserve.
- Financial Forecasting: Project how various claims scenarios would impact your bottom line, including best-case, expected, and worst-case scenarios.
- Risk Tolerance Assessment: Honestly assess your organization’s comfort level with financial uncertainty. Some businesses prioritize predictable costs over potential savings, while others are willing to accept some volatility for the opportunity to reduce overall expenses.
- Stop-Loss Affordability: Research stop-loss insurance costs for your specific situation. The premium expense needs to be factored into your overall financial analysis.
Long-Term Perspective: Self-funding typically delivers the greatest value over multiple years as employers gain experience and refine their approach. Consider whether your organization can commit to this strategy for the long term.
Evaluating Your Employee Population
The characteristics of your workforce significantly impact self-funded insurance viability:
- Population Size: Generally, larger employee populations (100+ employees) provide more statistical predictability for claims. Smaller groups face greater volatility risk, though innovative approaches like level-funding can mitigate this concern.
- Demographics Analysis: Assess the age distribution, gender mix, and family status of your employees. Younger populations typically present lower risk, while workforces with many older employees or dependents may experience higher claims.
- Geographic Concentration: Consider whether your employees are concentrated in regions with competitive provider markets or spread across areas with varying healthcare costs.
- Industry Factors: Some industries have inherently higher health risks due to physical demands or workplace conditions, which may impact self-funding suitability.
- Historical Claims Data: If available, analyze your group’s claims history to identify trends, high-cost conditions, and utilization patterns that might affect future costs.
Administrative Capabilities and Resources
Self-funding requires certain organizational capabilities:
- Benefits Administration Infrastructure: Assess whether you have staff with the expertise to oversee a self-funded plan or the budget to engage qualified external partners.
- Data Analysis Capacity: Consider your ability to analyze and act upon the claims data you’ll receive. This information is valuable only if you can use it effectively.
- Compliance Management: Evaluate your capacity to navigate the complex regulatory environment governing self-funded plans, including ERISA, HIPAA, and ACA requirements.
- Employee Communication Resources: Determine if you can effectively communicate plan changes and educate employees about how a self-funded plan works.
Vendor Management Experience: Consider your organization’s ability to select and manage relationships with TPAs, stop-loss carriers, and other service providers.
Decision-Making Framework
To systematically evaluate self-funding suitability, consider this step-by-step approach:
- Gather Information: Collect data on your current healthcare costs, employee demographics, and claims history (if available).
- Consult Experts: Work with experienced benefits consultants or brokers who specialize in self-funding to analyze your specific situation.
- Request Proposals: Obtain quotes from TPAs and stop-loss carriers to understand the actual costs for your organization.
- Conduct Financial Modeling: Compare projected self-funding costs (including administrative fees, expected claims, and stop-loss premiums) against fully-insured alternatives.
- Assess Implementation Requirements: Develop a realistic timeline and resource plan for transitioning to self-funding if you decide to proceed.
- Consider Hybrid Approaches: Explore intermediate options like level-funding or partial self-funding that offer some benefits of self-funding with reduced risk.
| Decision Factor | Consider Fully-Insured | Consider Level-Funding | Ideal for Self-Funding |
|---|---|---|---|
| Financial Stability | Unpredictable cash flow; limited reserves | Stable cash flow; moderate reserves | Strong reserves and consistent cash flow |
| Employee Population | Fewer than 50 employees | 50-200 employees | More than 200 employees |
| Risk Tolerance | Low tolerance for financial uncertainty | Moderate risk acceptance | Comfortable with managed risk |
| Administrative Capability | Limited benefits staff | Dedicated benefits personnel | Experienced benefits team |
| Claims Data | No claims history available | Limited claims data (1 year) | Multiple years of claims data |
Note: This is a simplified decision framework. Consult with benefits experts for guidance specific to your situation.
Making the Transition
If you determine that self-funded health insurance is appropriate for your organization, consider these implementation best practices:
- Start with Conservative Assumptions: Initially set aside more reserves than you expect to need until you establish a claims pattern.
- Implement Gradually: Consider a phased approach, perhaps starting with level-funding before moving to full self-funding.
- Prioritize Employee Communication: Develop a comprehensive communication strategy to help employees understand any changes to their benefits.
- Establish Performance Metrics: Define clear success metrics beyond just cost savings, such as employee satisfaction, health outcomes, and administrative efficiency.
- Plan for Continuous Improvement: Schedule regular reviews of your plan’s performance and be prepared to make adjustments as needed.
The decision to self-fund is significant but not irreversible. Many organizations find that the control, transparency, and potential savings make it worth the additional complexity and managed risk. By carefully evaluating your specific circumstances and implementing appropriate safeguards, you can determine whether self-funding represents the right strategic direction for your employee health benefits.
Frequently Asked Questions (FAQs)
Can Small Businesses Use Self-Funded Health Insurance?
Yes, small businesses can utilize self-funded health insurance, though traditionally it was more common among larger organizations. Today, innovative approaches like level-funding (a hybrid model) make self-funding more accessible to smaller employers. For businesses with fewer than 50 employees, careful consideration is necessary as the financial risk and claims volatility may be greater. Working with experienced benefits consultants and implementing appropriate stop-loss coverage are essential for small businesses exploring this option. Many small businesses start with level-funding arrangements, which combine elements of both self-funding and fully-insured plans, providing a lower-risk entry point.
What are The Legal Requirements For Self-Funded Insurance?
Self-funded health plans are primarily regulated by the Employee Retirement Income Security Act (ERISA), which establishes minimum standards for plan administration, reporting, and participant rights. Key legal requirements include:
- Filing Form 5500 annually with the Department of Labor
- Providing Summary Plan Descriptions (SPDs) to all plan participants
- Establishing claims and appeals procedures that meet federal standards
- Complying with applicable Affordable Care Act (ACA) provisions, including coverage for preventive services and essential health benefits
- Adhering to HIPAA privacy and security rules for protected health information
- Meeting Mental Health Parity requirements for behavioral health coverage
Self-funded plans are exempt from many state insurance regulations and premium taxes, which can provide significant administrative and cost advantages. However, employers must ensure compliance with all federal requirements to avoid penalties and legal issues.
How Do Self-Funded Plans Handle Catastrophic Claims?
Self-funded plans typically manage catastrophic claims through stop-loss insurance, which provides protection against unexpectedly high expenses. This insurance comes in two forms:
- Specific (Individual) Stop-Loss: Reimburses the employer when claims for any individual exceed a predetermined threshold (often $50,000 to $100,000, depending on group size and risk tolerance).
- Aggregate Stop-Loss: Provides protection when total claims across the entire plan exceed a specified percentage (typically 125% to 150%) of expected claims.
When catastrophic claims occur, the employer pays up to the stop-loss attachment point, after which the stop-loss carrier reimburses the employer for excess costs. Many self-funded plans also implement case management programs for high-cost conditions, centers of excellence for complex procedures, and second opinion requirements to help manage these expenses proactively.
Is Self-Funded Insurance More Affordable Than Traditional Plans?
Self-funded insurance can be more affordable than traditional fully-insured plans, but the answer depends on several factors specific to each organization. Potential cost advantages include:
- Elimination of insurance carrier profit margins (typically 3-5%)
- Exemption from state premium taxes (approximately 2-3%)
- Improved cash flow by paying claims as they occur rather than pre-paying premiums
- Direct access to claims data, enabling targeted cost-containment strategies
- Greater flexibility to customize benefits and implement innovative programs
However, self-funding also requires financial reserves to handle claims volatility and stop-loss insurance premiums, which can offset some savings. Organizations with younger, healthier employee populations typically realize greater savings than those with older or higher-risk workforces.
Studies suggest that well-managed self-funded health insurance plans can achieve 10-15% savings compared to equivalent fully-insured coverage over a 3-5 year period, though results vary significantly based on implementation quality and employee demographics.
Conclusion
Self-funded health insurance represents a powerful alternative to traditional fully-insured plans for many employers seeking greater control over their healthcare costs and benefits design. As we’ve explored throughout this comprehensive guide, self-funding offers numerous advantages, including potential cost savings, complete claims transparency, customizable benefits packages, and greater administrative control.
However, this approach isn’t without challenges. The financial risks, administrative complexities, and expertise requirements demand careful consideration before making the transition. Organizations must honestly assess their financial stability, employee demographics, risk tolerance, and administrative capabilities to determine if self-funding aligns with their specific circumstances.
For businesses with the right profile—stable finances, predictable claims patterns, and sufficient administrative resources—self-funding can transform healthcare from a frustrating expense into a strategic advantage. The ability to design plans that truly meet employee needs while potentially reducing costs creates a win-win scenario for employers and their workforce alike.
Even smaller organizations that traditionally might not have considered self-funding now have options through innovative approaches like level-funding and captive arrangements. These hybrid models offer many self-funding benefits with reduced risk exposure, making this approach more accessible than ever before.
Ultimately, the decision to self-fund requires thorough analysis, expert guidance, and a long-term perspective. While not suitable for every organization, self-funded health insurance deserves serious consideration as part of your benefits strategy. By weighing the pros and cons of self-funded health insurance outlined in this article against your specific business needs, you’ll be well-equipped to make an informed decision that supports both your financial objectives and your commitment to employee wellbeing.
References
- Employee Benefit Research Institute. (2023). “Self-Insured Health Plans: State Variation and Recent Trends by Firm Size.” Retrieved from https://www.ebri.org/health/publications/issue-briefs/
- U.S. Department of Labor. (2024). “Understanding Self-Funded Health Plans Under ERISA.” Employee Benefits Security Administration. Retrieved from https://www.dol.gov/agencies/ebsa/
- Texas Department of Insurance. (2024). “Employer self-funding of employee health benefits.” Retrieved from https://www.tdi.texas.gov/pubs/consumer/cb108.html
- Kaiser Family Foundation. (2023). “Employer Health Benefits Annual Survey.” Retrieved from https://www.kff.org/health-costs/report/employer-health-benefits-annual-survey-archives/
- Society for Human Resource Management. (2024). “Self-Funding: Considerations for HR Professionals.” Retrieved from https://www.shrm.org/resourcesandtools/
- American Academy of Actuaries. (2023). “Emerging Data in Self-Funded Health Plans: Risk and Reward.” Retrieved from https://www.actuary.org/
- International Foundation of Employee Benefit Plans. (2024). “Self-Funding Health Benefit Plans: Employer Perspectives.” Retrieved from https://www.ifebp.org/
- Health Care Administrators Association. (2023). “Self-Funding Fundamentals for Plan Sponsors.” Retrieved from https://www.hcaa.org/
- Business Group on Health. (2024). “Trends in Self-Funded Health Plans Among Large Employers.” Retrieved from https://www.businessgrouphealth.org/
- Self-Insurance Institute of America. (2023). “The Self-Insurance Protection Act: Implications for Employers.” Retrieved from https://www.siia.org/