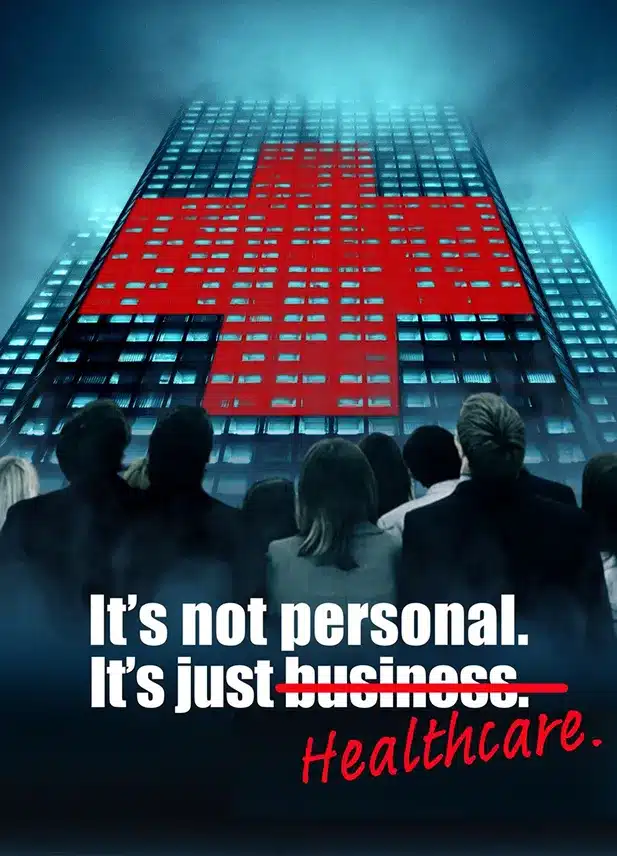
What Happened...
What it's really about...
Here's where we shed some light...
In light of these developments, Ethos Benefits conducted a comparison of the drugs mentioned in the lawsuit and found significantly lower costs available to their employer clients (more on that below). This underscores the importance of thorough oversight and negotiation when it comes to healthcare contracts. Employers must ensure that they are getting fair value for their healthcare spending and that employees are not unfairly burdened with excessive costs.
So, what can employers do to navigate these complex waters? One key step is establishing a health and welfare benefits committee that monitors ERISA benefits, reviews contracts and ensures cost-effectiveness. This committee plays a crucial role in upholding fiduciary responsibilities and protecting employees’ interests.
Additionally, employers should consider implementing fiduciary training, reviewing insurance policies, and negotiating indemnification provisions with service providers. Ethos Benefits offers valuable resources and guidance to help employers navigate these challenges effectively.
In conclusion, the J&J lawsuit serves as a wake-up call for employers to prioritize transparency, fairness, and prudent decision-making in managing their employees’ healthcare benefits. This is something we take seriously and is the core component of our business model since our inception. Reach out to us and we can help ensure compliance, minimize risks, and ultimately provide better healthcare outcomes for your employees.
Bonus: If you’re now wondering about the cost of your medications, send your broker the list below of the 35 drugs we completed the comparison with and then ask them the cost.